Epiretinal membrane
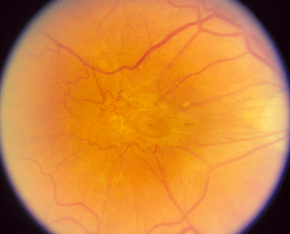
An epiretinal membrane is a thin layer of scar tissue that can develop on the surface of the macula at the centre of the retina and cause a disturbance in vision. An epiretinal membrane is also sometimes called a macular pucker or cellophane maculopathy.).
In the majority of cases, an epiretinal membrane develops in an eye with no history of previous problems. This type of epiretinal membrane is called idiopathic. Occasionally however, an epiretinal membrane will develop in the eye as a result of retinal detachment, trauma, inflammatory disease or retinal blood vessel abnormalities. Most epiretinal membranes are mild and have little or no effect on vision. However, in some cases, the epiretinal membrane may slowly grow and contract which can cause mechanical distortion (“wrinkling”) in the macula. This may lead to blurred or distorted vision, which may slowly worsen over time. An epiretinal membrane does not make an eye go completely blind but it typically affects the centre of the of the vision and does not affect peripheral vision.
Management
Not all epiretinal membranes require treatment. Surgery is not necessary if the epiretinal membrane is mild and having little or no effect on vision. If the epiretinal membrane is causing significant distortion or blurred vision however then vitrectomy surgery is the only way of improving vision.
The surgery consists of making three tiny incisions in the white part of the eye (the sclera) . The vitreous gel is first removed and then the membrane is peeled from the retina using microforceps. I use small 25 guage instrumentation which means that the wounds self sealing and in most cases do not require sutures. This means that the eye recovers more quickly from the surgical procedure.
Results
Most patients will have a significant improvement in vision after surgery, however this may occur gradually over several months. The amount of visual improvement varies from person to person and depends on multiple factors including the severity and chronicity of the epiretinal membrane, the level of vision preoperatively, and the presence of any other ocular abnormalities. Typically 90% of patients will notice an improvement in distortion and 80% of patients will have an improvement in vision.
Any surgical procedure carries a risk of complications and epiretinal membrane surgery is no exception. Post-operative infection (endophthalmitis) can be very serious and may lead to blindness in the affected eye. Most infections can be effectively treated if identified at an early stage. Endophthalmitis is rare and occurs in approximately 1 out of 2000 cases. Retinal detachment is another complication that can cause blindness if not treated. Retinal detachments occur in 1 out of 100 cases following epiretinal membrane surgery. The progression of cataract is a third consideration. A cataract occurs when the lens in the eye becomes cloudy and typically occurs with aging but is accelerated by vitrectomy surgery. If there is any degree of cataract before the vitrectomy, I tend to combine the vitrectomy procedure with cataract surgery to avoid a second procedure and speed visual rehabilitation.
For more information see: www.beavrs.org


